Winter redness flare-ups are super common. Cold wind, indoor heating and rapid temperature shifts place extra stress on reactive skin, often triggering flushing, heat and sensitivity across the cheeks and nose.
The goal is control, not “stripping back”. Focus on reducing redness while keeping the skin barrier intact with gentle, consistent skincare, practical trigger management, and evidence-based options you can discuss with a clinician.
What is rosacea?
Rosacea is a long-term tendency towards facial redness and sensitivity, most often affecting the cheeks, nose, chin and forehead. It can present as frequent flushing, persistent background redness, visible fine blood vessels, and a burning or stinging sensation. For some people, it also includes spot-like bumps that can be mistaken for acne.
It’s not caused by poor hygiene. In fact, aggressive cleansing and over-exfoliation are common reasons symptoms intensify, because they disrupt the skin barrier and make reactive skin harder to settle.
What to avoid in winter
Avoid products that are likely to inflame reactive skin or disrupt your skin barrier. Fragrance is a common issue, including essential oils and strong menthol or camphor “tingly” formulas that can feel soothing at first but often worsen redness over time.
Physical scrubs, cleansing brushes, and frequent exfoliation are also common triggers, particularly in cold weather when your skin barrier is already under strain.
During a flare, be cautious with acids and heavy routines. Overuse can increase stinging, dryness, and rebound sensitivity.
Finally, avoid using steroid creams on facial redness without medical supervision, as they can cause dependency and may worsen symptoms once stopped.
Rosacea subtypes, and why yours matters
Rosacea presents in a few distinct patterns. Identifying your dominant subtype helps you choose an approach that is more targeted, more tolerable, and less likely to aggravate the skin barrier.
Erythematotelangiectatic rosacea (ETR)
This is the classic flushing pattern. You may notice frequent blushing, persistent background redness, and visible fine vessels.
Papulopustular rosacea
This subtype includes inflamed bumps and pustules alongside a baseline of redness. It’s often confused with acne, but rosacea tends to lack blackheads and usually comes with flushing and sensitivity as the underlying theme.
Ocular rosacea
This affects the eyes rather than just the skin. Symptoms can include dryness, grittiness, watering, irritation, or sore eyelids. If you suspect ocular rosacea, it is best to seek medical advice rather than self-treating.
Phymatous rosacea
A rarer subtype where skin texture becomes thicker or more irregular, most commonly around the nose. Early assessment is important, as management is more effective when addressed promptly.
Why winter makes rosacea worse
Winter places multiple, overlapping stresses on reactive skin. Together, they make flare-ups more likely and harder to calm if the skin barrier is already compromised.
Cold air and wind weaken the skin’s protective barrier, increasing dryness and sensitivity. Indoor heating then adds to the problem by lowering humidity, which can worsen dehydration and trigger stinging or tightness.
Moving between cold outdoor air and warm indoor environments can add another challenge, often causing sudden flushing. UV exposure also remains relevant in winter, even on overcast days, which is why daily SPF is super important in rosacea management.
Common rosacea triggers
There is no universal trigger list, but a few patterns appear again and again in winter flare-ups. The most common include cold wind and temperature shifts, heat exposure, spicy foods, stress, intense exercise, sun exposure, and skincare irritation.
Alcohol can also be a driver for some people. Red wine and spirits are frequent culprits, often because they combine vascular effects with histamine sensitivity.
If your triggers are not obvious, keep it simple. Track flare-ups for two to three weeks and note the basics in the 24 hours beforehand: weather exposure, food and drink, stress levels, exercise, and any new skincare. A short, consistent diary is usually enough to reveal the dominant pattern.
What to avoid in winter
Avoid products that are likely to inflame reactive skin or disrupt your skin barrier. Fragrance is a common issue, including essential oils and strong menthol or camphor “tingly” formulas that can feel soothing at first but often worsen redness over time.
Physical scrubs, cleansing brushes, and frequent exfoliation are also common triggers, particularly in cold weather when your skin barrier is already under strain.
During a flare, be cautious with acids and heavy routines. Overuse can increase stinging, dryness, and rebound sensitivity.
Finally, avoid using steroid creams on facial redness without medical supervision, as they can cause dependency and may worsen symptoms once stopped.
Evidence-based options to discuss with a clinician
Rosacea is very dependent on your own personal skin type, so the right plan depends on your subtype, your sensitivity level, and what your skin is doing right now. A consultation helps us choose options that support results without upsetting your barrier.
Topical treatments for rosacea (at-home, clinician-guided)
Depending on your symptoms and skin tolerance, we can recommend topical treatments such as azelaic acid, metronidazole, or ivermectin cream.
Light-based and supportive options (clinic-led)
If your main concern is persistent redness, flushing, and visible vessels, light-based treatments can be worth discussing. The aim is to improve the appearance of redness and thread veins while keeping your skin calm and comfortable.
IPL is commonly used to help improve uneven skin tone, reducing the appearance of thread (spider) veins and redness for suitable candidates. It can be a helpful option when “background redness + visible vessels” is a key feature, but results vary and it isn’t right for everyone — especially if your skin is actively flaring or very sensitised.
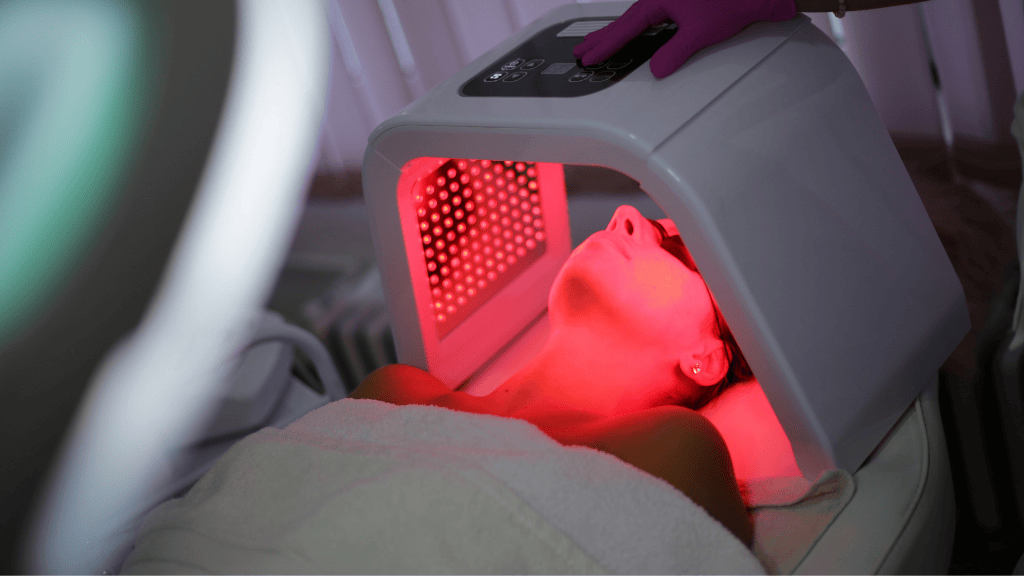
Dermaux LED
DermaLux uses wavelengths of red, blue and infrared light delivered at specific depths to support skin health and help calm skin that’s easily triggered by environmental stressors.
Many people find LED a comfortable supportive option alongside a barrier-first routine, particularly in winter when skin feels more reactive.
HydraFacial
HydraFacial is a treatment designed to refresh the look and feel of skin through cleansing and hydrating the skin. During this treatment we’ll focus on comfort and tailor the settings and ingredients carefully to avoid overstimulation.
Advanced Skin Care
Our team is here to guide you towards advanced skincare products that suit your skin type and tone.
Visit our clinic in Weybridge where we offer bespoke advanced skincare treatments to improve the health of your skin for a more refreshed, brighter complexion.
How Light Touch Clinic can help
At Light Touch Clinic in Weybridge, Surrey, we take a barrier-first approach to facial redness. We identify what is driving your symptoms, review your current routine, and set a plan that is realistic to follow.
For many patients, that starts with simplifying skincare and rebuilding tolerance. Where appropriate, we may also recommend a medical-grade programme such as ZO Skin Health, selected to support the skin barrier while targeting redness-prone behaviour. If you are a suitable candidate, we can also discuss clinician-led options such as IPL, LED Light Therapy or Hydrafacial.